There are no products in your shopping cart.
Post exertional malaise, activity and mitochondrial myopathy.
Sat, 02/13/2010 - 12:33am
There is a new blog entry on www.cfsandxmrv.blogspot.com on ME/CFS and post exertional malaise, a rather delacate and sensitive topic. Feel free to have a look, leave a comment, and please share with family, friends, and the medical community. The more education we get out there, the better.
Regards, ek
This forum is provided to allow members of Lumigrate to share information and ideas. Any recommendations made by forum members regarding medical treatments, medications, or procedures are not endorsed by Lumigrate or practitioners who serve as Lumigrate's medical experts.


![Expand cart block. []](/sites/all/modules/ubercart/uc_cart/images/bullet-arrow-up.gif)


I happened to see this link posted in a group about CFS/FM on Facebook and thought it was a good little documents to add into the forums on Lumigrate. The people in the group had made several comments that indicated it was of interest to them. I wasnt sure if any of them had looked at the PDF or not, or were just commenting off of what the poster, the group's creator and admin, had said as she gave a good setup of what the document provided in general.
I got the impression that people are still feeling the 'need' to have 'evidence' to show others that CFS is a disorder that truly affects the body and not one of 'the mind's creating this, it's made up in your head'. Which is really too bad because there has been ample evidence even just here at Lumigrate that people have access to finding their way to, that should make that very clear. It takes open minds PLUS education or somehow figuring something out to change opinions.
So here's something that's a good 'supportive evidence document' if you're interested. I was pleased to see that Emma-Kate's link still works to go to that topic at blogspot dot com -- she was providing amazing information and I was so proud to have her register as a user and post a little at Lumigrate so other seekers could find her blog. The same for the woman who posted this link, she had registered and posted early on at Lumigrate so that people can find her too, from the forums at Lumigrate.
www.translational-medicine.com/content/pdf/1479-5876-12-20.pdf
Abstract from the document:
Background: The insufficient metabolic adaptation to exercise in Chronic Fatigue Syndrome (CFS) is still being
debated and poorly understood.
Methods: We analysed the cardiopulmonary exercise tests of CFS patients, idiopathic chronic fatigue (CFI) patients
and healthy visitors. Continuous non-invasive measurement of the cardiac output by Nexfin® (BMEYE B.V.
Amsterdam, the Netherlands) was added to the cardiopulmonary exercise tests. The peak oxygen extraction by
muscle cells and the increase of cardiac output relative to the increase of oxygen uptake (ΔQ’/ΔV’O2) were
measured, calculated from the cardiac output and the oxygen uptake during incremental exercise.
Results: The peak oxygen extraction by muscle cells was 10.83 ± 2.80 ml/100ml in 178 CFS women, 11.62 ± 2.90 ml/
100 ml in 172 CFI, and 13.45 ± 2.72 ml/100 ml in 11 healthy women (ANOVA: P=0.001), 13.66 ± 3.31 ml/100 ml in
25 CFS men, 14.63 ± 4.38 ml/100 ml in 51 CFI, and 19.52 ± 6.53 ml/100 ml in 7 healthy men (ANOVA: P=0.008).
The ΔQ’/ΔV’O2 was > 6 L/L (normal ΔQ’/ΔV’O2 ≈ 5 L/L) in 70% of the patients and in 22% of the healthy group.
Conclusion: Low oxygen uptake by muscle cells causes exercise intolerance in a majority of CFS patients, indicating
insufficient metabolic adaptation to incremental exercise. The high increase of the cardiac output relative to the
increase of oxygen uptake argues against deconditioning as a cause for physical impairment in these patients.
Keywords: Chronic fatigue syndrome, Exercise test, Exercise intolerance, Oxygen extraction
Background from the document
Background
Exercise intolerance is a frequent complaint from patients
who meet the criteria for Chronic Fatigue Syndrome/
Myalgic Encephalitis (CFS) and Idiopathic Chronic Fatigue
(CFI) [1].
Objective tests for physical impairment measure the
maximal oxygen uptake (peak V’O2) during a cardiopulmonary
exercise test (CPET) [2-4]. Most studies agree
that peak V’O2 is lower in CFS, but we need to understand
the cause of the lower peak V’O2 to explain the
pathogenesis.
The V’O2 depends on the uptake, transport and metabolism
of oxygen in the muscle cells during physical
exercise. In most CPET studies in CFS patients, the limitation
of peak V’O2 is not attributed to a lower uptake
and transport of oxygen to the muscle. A lower metabolic
capacity of the muscle cell would change the demand
for oxygen and thus lower the oxygen extraction
(C(a-v)O2) and increase the cardiac output relative to
V’O2 (ΔQ’/ΔV’O2) [5,6]. In previous studies we, and
others, did not find impaired mitochondrial activity to
be a cause for a lower peak V’O2 [4,7], but abnormal mitochondrial
activity was reported by some in CFS and CFI
[8-10].
The aim of the present retrospective study was to determine
to what extent the physical impairment in CFS
and CFI was attributable to changes in uptake, transport
and metabolism of oxygen in the muscle cells.
Conclusions from the document, and their citing specifications (is open access):
CPET with continuous measuring of cardiac output by
Nexfin allowed for the calculation of the presence and
severity of metabolic causes of exercise intolerance. This
retrospective study showed that a low oxygen extraction
and a high ΔQ’/ΔV’O2 were consistent with a metabolic
cause for exercise intolerance in 70% of CFS patients.
Cite this article as: Vermeulen and Vermeulen van Eck: Decreased
oxygen extraction during cardiopulmonary exercise test in patients with
chronic fatigue syndrome. Journal of Translational Medicine 2014 12:20.
Live and Learn. Learn and Live Better! is my motto. I'm Mardy Ross, and I founded Lumigrate in 2008 after a career as an occupational therapist with a background in health education and environmental research program administration. Today I function as the desk clerk for short questions people have, as well as 'concierge' services offered for those who want a thorough exploration of their health history and direction to resources likely to progress their health according to their goals. Contact Us comes to me, so please do if you have questions or comments. Lumigrate is "Lighting the Path to Health and Well-Being" for increasing numbers of people. Follow us on social networking sites such as: Twitter: http://twitter.com/lumigrate and Facebook. (There is my personal page and several Lumigrate pages. For those interested in "groovy" local education and networking for those uniquely talented LumiGRATE experts located in my own back yard, "LumiGRATE Groove of the Grand Valley" is a Facebook page to join. (Many who have joined are beyond our area but like to see the Groovy information! We not only have FUN, we are learning about other providers we can be referring patients to and 'wearing a groove' to each other's doors -- or websites/home offices!) By covering some of the things we do, including case examples, it reinforces the concepts at Lumigrate.com as well as making YOU feel that you're part of a community. Which you ARE at Lumigrate!
I've taken a comment I left on the above PDF in the group I was referring to and edited it a bit to become a comment here on Lumigrate.
Great data to support what providers who know how to address this have been doing for years and decades. Dr Teitelbaum's SHINE protocol has E for exercise and he has long published and presented even on TV about the underlying reasons for the symptoms patients with fatigue experience. And many others.
There is no lack of info, it's the consumers and then providers finding the same things so they can group up and get a treatment plan in place is the trick. The consumers today know more about what they need help with from providers than the providers, who have dizzying responsibilities and tasks taking time as the health care system is in such transition now. Very unfortunate, as this does not have to end up for people as it often does. So, great to see this document that inspires people here!
In the mid 2000's, I had developed a system of teaching patients mindfulness meditation and deep breathing, and about hydration, on day #1 after evaluation (it is/ was required by insurance you do treatment on day of eval). This was based on melding my OT experience with my personal experience having had CFS and FMS diagnosed in my past and having made a good reversal of symptoms.
Without exception, the patients who found their way had good results, and they would get rapidly transferred to PT to progress them along longer term, so in OT we could focus on function. And this was in conventional medicine, they were typically not going to doctors or other providers who know about nutrition and supplementation and etc.
Some had been too low stamina and energy to participate in desired pool therapy, as it took too much energy to get there and showered and redressed and home.
And a ripple effect happened, because therapists of all sorts simply needed to look at activity level and where to start and how to bill for a 45 minute session different than their recipe is for ortho or other neuro patients who had more energy. Even the more knowledgeable did not really understand that the energy level is similar to when you're laid out with the influenza -- in some people. (Naturally there are some that bedridden and would need the professionals coming to them in the home.)
Fortunately, i knew from one job working for medical sharks for a short time (I resigned my second day but gave notice so they could replace me) that it would fly okay to bill for time teaching meditation. (Proving the silver lining in perhaps every difficult situation I've encountered in life, maybe others can see this as well -- 'everything has a reason' .... Just something to think about!)
I would also document why i chose to do that on day one, in a way that any reviewer would understand it. And it was as much to do with them developing their ability to monitor what was right for them .... your gut some might say. Putting them in control of their wellness if they did not feel that or see it that way. Because how long and what activity one does changes from day to day and even moment to moment.
We also learned to not expect to do more the next day and on and on as is the conventional way we were taught to exercise. Monitor and do what you think is right which supercedes what I or any provider says. We are just people hired to help advise.
Then day #2 of therapy, usually 2-3 days later, we'd review that after talking about how they felt after and if they'd practiced their 'homework' of breathing / meditation (and hydration), and go to the gym with our water bottles. We'd pick up to 3 pieces of equipment .. arm bike, leg bike, treadmill, eliptical, stairmaster. Then they did up to 2 minutes, very slowly, easily.
They were congratulated equally if it was 2 seconds or 2 minutes they went for as long as they monitored their fatigue. The recognition was for doing an appropriate amount, not doing some preconceived or 'wished for' / desired / 'expected' amount. You'll see here reading between the lines, you're teaching people to be in the moment, go with the flow. Then they'd breathe and relax, sip water, and if they felt they could and should, do a second type of equipment. Etc.
3rd day of therapy, we'd repeat the performance and based on how they felt after they left therapy, they (with my input) figured out what to do that day with the equipment.
And then we started transitioning to get PT ordered. The PT (which was one of two in our clinic, that had agreed to taking patients with CFS/ FMS -- they're overall a difficult group to treat that provides frustrations to some PTs, particularly those who went into the field due to their interest in athletic training, but that was not always the case). And they'd take it from there, with me right around all day if they had any questions or wanted input or feedback on how the patient was doing. At that clinic we weren't given the opportunity to do a collaborative care meeting weekly unless we took it out of our personal time, which is not allowed by Federal labor laws so we just kept it informal. I continued to meet with the PhD psychologist in his office once a week because I worked for myself as did he so we could set our policies. Later he and I would help startup a new clinic based on the collaborative care model, which was marginally successful for the first year that the original team was still interested in being part of the clinic but it rapidly (even before opening officially) turned into a different reality than what we'd discussed beforehand. Again, due to the ownership/ management decisions.
It was not our business, we were renters or involved ad hoc so it went differently than we'd envisioned. So unfortunately the progression of a program to do this kind of work did not happen for me at that time and I'm left with writing about it about the past and looking forward to perhaps helping create things like this elsewhere for other clinics and communities.
The PTs could also do the usual helping for aches and pains, which was great. And refer to the MT in house, who could technically be doing PT Aide work and doing soft tissue work on the patients. This was complex in terms of communication with the schedules and it was not done as often as I had hoped. It was a great MT, and I have the ultimate respect for a good MT being on the team a patient gets surrounding them. (See the Lumigrate model).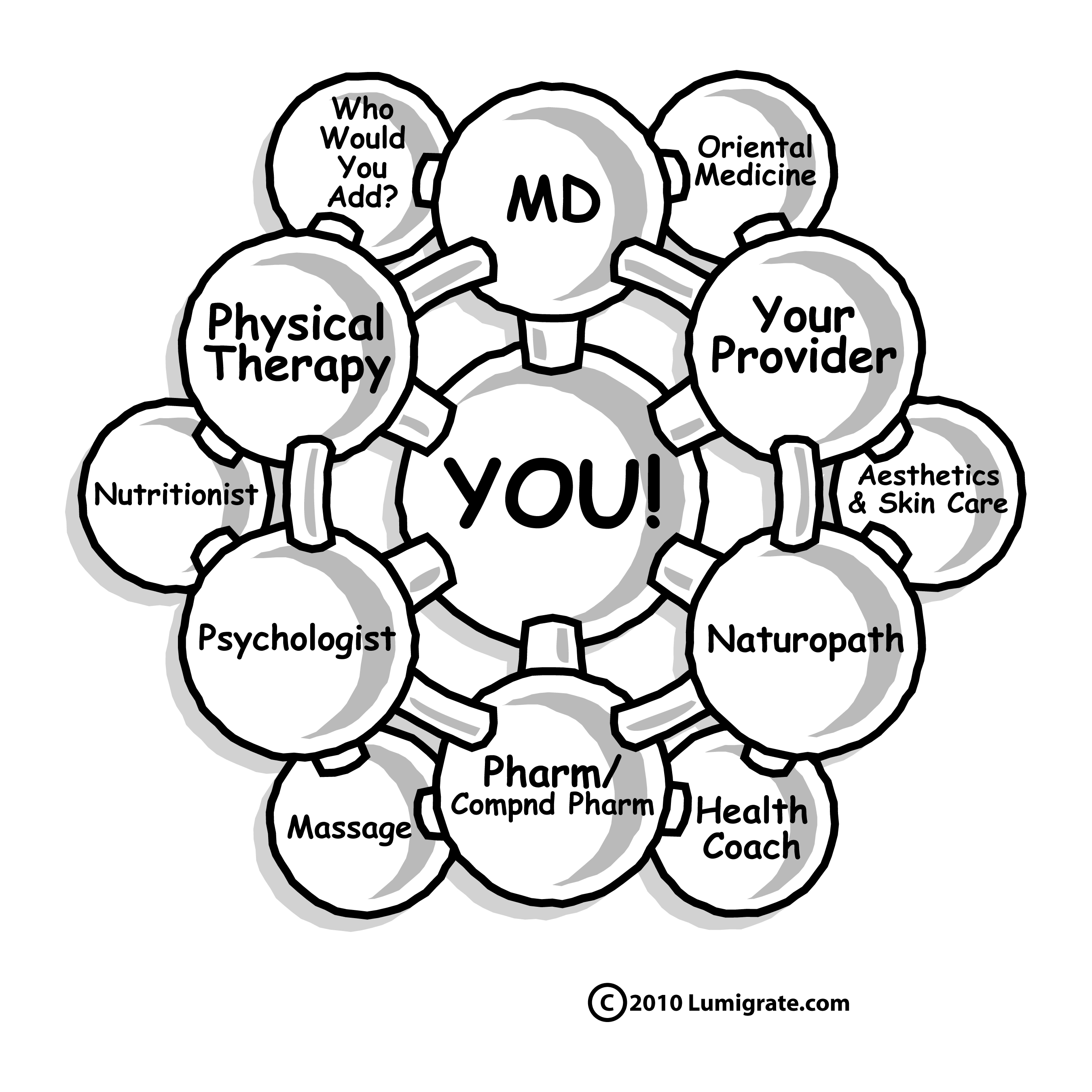
They were also referred to the buildings pain mgmt psychologist, whom I met with every week to discuss our mutual patients, and then I'd pass info from the PTs and him back and forth if pertient -- this way we really understood the patient and kept them in the loop that we were doing this on their behalf. It's very impressive to them that they're considered so highly that we'd do all that! As it should be, they're coming to us, entrusting us to help them.
If they wished to see the behavioral health specialist (2 floors above us in the building), after I explained what they did with a book he wrote about pain mgmt, plus a great muscle biofeedback program they had. Or he'd refer people to me and then I'd get them set up to succeed with PT. Soon the PTs didnt need me priming the patients, they had the recipe. Maybe someday what I did there will catch on. I even revised the book at one point and used it with my patients and it was very helpful to them. Many would not be able to see the PhD in our building due to insurance reasons or they already had a provider of that type and didn't want to change 'ships', but wanted the additional information. We really were helping a good number of people.
Most said on their first intake day/ evaluation interview that they had PT ordered in the past and they went and were flared up so didnt go back. And they just no showed.
Which is why the clinic I was at initially didnt want me to start a program for people with FM, they'd messed up the clinic's productivity (which is in all therapists contracts or written job expectations to bill for a certain % of time), and by no showing when it was not forgetting or confusion were being unacceptable for that clinic. What was neat in retrospect as time went forward is they'd gotten over that and even created a program about veterans and brain injury and were doing special procedures to be sure they were handled well due to their memory problems and their difficulties with route finding as they had to come into the building and get on an elevator and go to a certain floor and get off and find the clinic and it was a very confusing buildng the way the interior was designed.
They certainly had made it more like a hotel look than a medical building where people with damaged and mis-functioning brains would be trying to find their way around. (I had a friend who knew medical building construction come to the office once and he said that they didn't hang the doors the direction you would a medical building so that the patient is kept shielded by the opening door, something I'd long since forgotten from a past interest in functional architecture and design). So in other words the PT department of this building essentially had figured out what they needed to do to help the type of patients who have CFS/ME and FM, etc. Progress!
Initially when I was there trying to get this program together for the CFS/FMS etc population off the ground, by explaining to the therapy management who did not know that many who get CFS and FMS had dysfunctional families of origin (and maybe since) which lead to them not feeling empowered to make needs known and to be empowered enough to simply call up and say 'your therapist hurt me, i am cancelling my appointment', it was helpful to have this information come to light. Until one studies the data about people who get CFS / FMS one does not know that, and PTs don't get much psychology training same as OTs don't get much training about things PTs are 'THE therapist' for.
Learning how I, as an OT, could bill for that type of therapy (giving them the % of revenue required to be there within their group), it became a money maker for all involved and, as I said, without exception, our patients had improvements. (And for UEs you do the same things you would for patients who have had strokes and do 1# dumbells if needed to start, up to 2 then 3 and so on... not 5 or 10 to start, and maybe never get to those.)
It's an energy crisis in the muscles and all tissues, the "mighty mitochondria" problem needs to be addressed ideally, and that requires other providers and was where it got tricky for those who only could or wanted to use insurance. The people who could advise about that were not insurance based. (We have information about these things on Lumigrate, I suggest you seek them out with the Search bar here. Dr Spurlock's forum in this section about FMS / CFS has much information as do the other topics in this forum and many others).
But those providers who knew about what would help people because they treated many people successfully with CFS FMS who were paying out of pocket gladly would come speak to the education group we started (free marketing, they're always on a budget for marketing expenses and education groups are great places to get new customers). Also, when we didn't have a guest speaker, the people who came who paid to go to the competent advisors about that (and who also did online or book research) would share what they knew and then it was a matter of the lower funds folks figuring how to get supplements and improved nutrition. And they were there before the providers started coming -- it was THEIR GROUP -- so they felt empowered to speak up if there was something they knew they could add. We had good discussions and there were "Aha moments" that happened for providers and consumers/ patients with fatigue and pain, alike!
We had to stop that when it got off the ground because I had moved on to the aforementioned integrative clinic to create, in part, a website to bring info to people since more people could not attend meetings than could. Which became Lumigrate (dot com), this website. Which, since 2009 has been collecting different resources for those that find their way there. For well wanting to stay that way, or ill wanting to get things turned back around towards wellness.
Just this weekend I was talking with someone who was disabled from the overlapping conditions who had been realizing how much exercising -- the way she does it -- helped her recover a lot. (Writing this on Tuesday morning after Labor Day weekend.) This is a woman who identifies with the Lyme aspect of the overlapping conditions and has learned much about how vaccines play into the contributing factors, which is her area of activism.
Monday evening I spoke with someone who had "the stuff" come on fairly suddenly in early 2013 and got turned around fast once they contacted me and i could suggest who to go to for advise as they were misdirected by their primary care. They talked of a very active weekend and the usual fall busyness for work and school and they realized their crash was somewhat to do with having not exercised when their time was overbooked. So now they 'pace' and prioritize and won't drop exercise time out again. Which they figured out by being 'tuned in' as a long-time meditator. So having access to just checking in with the team-mates they have put around them on their health care team, infrequently as long as they're doing well, is something that is helpful support to them, which has not existed up until now that I'm aware of, in the insurance-based allopathic medicine model in the US.
Obviously, important also is sticking to a diet where they see good results, in this person's case it is admitted to be not "ideal" but they're finding those balance points as they continue month after month recovering from a sudden massive crash of their wellness (late, it happened when they were over 50 which is a little on the older end for when I typicallyl see people having their health fall apart but that is the 'new normal', we're seeing more having it occur younger too -- just increasing toxic 'load' of many things affecting body, mind, spirit).
And they stick to their vaccine plan now and don't make decisions hastily when in the presence of those whose job it is to encourage mass vaccinations. 2 falls ago they felt pressure to get a vaccine just before, but they see it was that, this, the other combined. They had not previously studied why it is that some people have problems and naturally we have information about that, which this person has had access to like anyone else, to study if they wish. It tends to be that the more a person applies themself to studing any issue, the more they navigate in the future in an improved way.
And that is what recovery takes a course of up and down typically, and it's a long process; there are many facets to address. This is hard to do when you're not well sometimes, as it's a catch 22... your brain's affected and the key to putting a plan together and carrying it out. Most of it can be DIY if people have the info and some support. So in closing that is why I suggest if people cannot do it on their own they recruit someone to help them learn and navigate, a patient advocate in the form of a friend, family member or otherwise.
For what it's worth, that is the history of what I can summarize was my professional 'success' with this type of patient, both face to face in an insurance-based allopathic model, and after that in advising people about what education to seek out about various types of providers and teaching patients to become proactive consumers in a difficult to navigate medical environment, using their resources of time, energy and money (insurance for those who had it falls under that category, or their copay or if they pay entirely out of pocket).
Live and Learn! Learn and Live Better!! ~ Mardy
Live and Learn. Learn and Live Better! is my motto. I'm Mardy Ross, and I founded Lumigrate in 2008 after a career as an occupational therapist with a background in health education and environmental research program administration. Today I function as the desk clerk for short questions people have, as well as 'concierge' services offered for those who want a thorough exploration of their health history and direction to resources likely to progress their health according to their goals. Contact Us comes to me, so please do if you have questions or comments. Lumigrate is "Lighting the Path to Health and Well-Being" for increasing numbers of people. Follow us on social networking sites such as: Twitter: http://twitter.com/lumigrate and Facebook. (There is my personal page and several Lumigrate pages. For those interested in "groovy" local education and networking for those uniquely talented LumiGRATE experts located in my own back yard, "LumiGRATE Groove of the Grand Valley" is a Facebook page to join. (Many who have joined are beyond our area but like to see the Groovy information! We not only have FUN, we are learning about other providers we can be referring patients to and 'wearing a groove' to each other's doors -- or websites/home offices!) By covering some of the things we do, including case examples, it reinforces the concepts at Lumigrate.com as well as making YOU feel that you're part of a community. Which you ARE at Lumigrate!