There are no products in your shopping cart.
The Differences Between Women and Men in Diagnosing and Treating Their Chronic Pain and Illnesses
Women and men are treated very differently by the allopathic, conventional medicine system when it comes to diagnosing and treating pain, as this recent piece by Laurie Edwards so brilliantly conveys in the New York Times (dot com, online version, links included and encouraged to go read at the source for all the fun images, etc.).
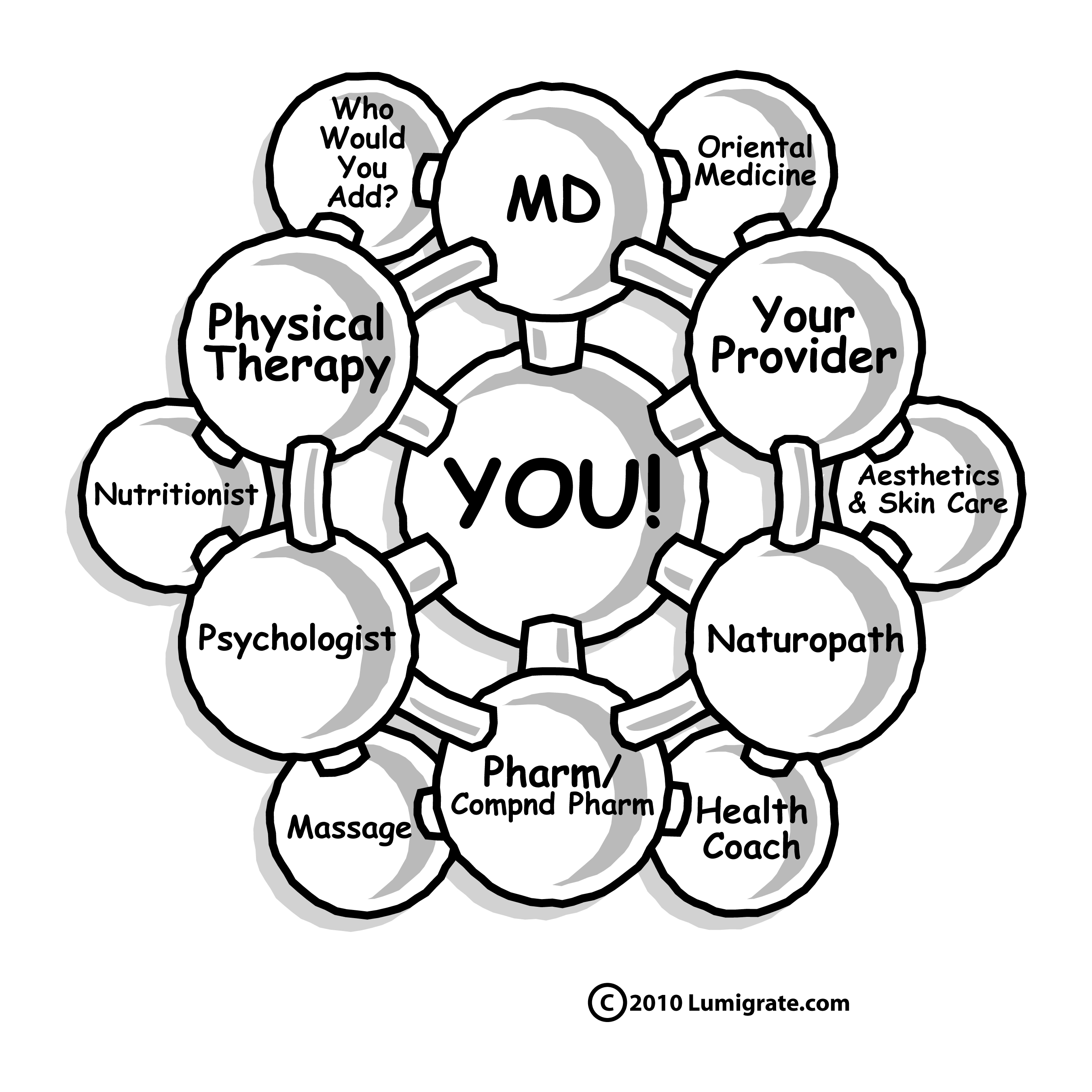
I recommend men and women read this, whether you have chronic pain and chronic illness or if you're one who has chronic wellness and don't have pain as part of your typical daily existence: this affects EVERYONE directly or indirectly. Again, it gets to the Lumigrate YOU! Model, and changing your health care system surrounding you NOW, as much as possible, in order to increase your well-being as much as possible.
I call it "health care reform from the inside out", or when I spoke with Alan Phillips, J.D. recently when he was adding himself to be part of our expert team at Lumigrate related to vaccine law and legal rights, when he viewed the model for the first time he saw it as 'from the bottom up approach' as opposed to the top down, the way the allopathic model does.
The only point I'd like to pull out and highlight here related to the statistics Ms. Edwards sites is related to the numbers stated for having fibromyalgia or having chronic pain: These are always low, because the information out there is based on information given by people who have been identified or who self-identify as having something to report.
I have heard environmental medicine specialst Wm. Marc Spurlock, MD state that 20% of the US population right now experiences the symptoms of chronic illness/chronic pain that falls on the 'spectrum' of chronic fatigue/fibromyalgia, and that the number is rapidly growing because of all the factors people are exposed to in the United States in our current times, and that if 'we' don't make the changes collectively and individually to turnaround the trend, it would end up with virtually everyone being on the chronic illness end of the continuum and not on the chronic wellness side of the dividing line.
The most recent statistics I found recently about the overall chronic illness rate was that 50% of Americans are diagnosed with at least one of the chronic illnesses. Again, this does not factor in those who are unaware they have diabetes or fibromyalgia or hypothyroidism, etc.
When I first looked into these statistics in detail, in 2007 when considering creating what you now see as Lumigrate.com, which is four years on the Internet as of this week, the data available stated the rate was 2004, so essentially in 2-3 years time the numbers jumped 10%! And the data tends to be from several years prior. I worked in research offices at a major University from 1979 to 1992 and understand well why it takes a while to collect data, crunch it, analyze it, write it up, produce it and get it 'published' where people start being able to utilize it in their work, as Ms Edwards has or any of us who are working to find and report on what is going on and 'get the word out' to people and be part of the changes that are occurring, thankfully, in recent years.
So please read this article, shared in full below but with the link underneath to go view it at it's source if you wish, and also spend a moment reflecting upon if you or someone close to you has symptoms of what might be a chronic illness that would be of benefit for you or them to address. Or if you're seeing details in this related to the treatment of insomnia (Ambien is noted here) or pain which might be of benefit for someone you know to read, please share with them; this includes your medical providers. There is a virtual army of educators to help the providers get the information which is 'really important'; in effect one person turning a provider onto this type of information can change how thousands of people are treated. Wouldn't THAT be something YOU can do to 'reform' health care today?
The Lumigrate YOU! Model:
HOPE
{BOLDING, below, added by me for the ease and streamlining of Lumigrate's typical education-seeking guest}
The Gender Gap in Pain
Women have hormonal cycles, smaller organs, higher body fat composition — all of which are thought to play a role in how drugs affect our bodies. We also have basic differences in gene expression, which can make differences in the way we metabolize drugs. For example, men metabolize caffeine more quickly, while women metabolize certain antibiotics and anxiety medications more quickly. In some cases, drugs work less effectively depending on sex; women are less responsive to anesthesia and ibuprofen for instance. In other cases, women are at more risk for adverse — even lethal — side effects.
These differences are particularly important for the millions of women living with chronic pain. An estimated 25 percent of Americans experience chronic pain, and a disproportionate number of them are women. A review published in the Journal of Pain in 2009 found that women faced a substantially greater risk of developing pain conditions. They are twice as likely to have multiple sclerosis, two to three times more likely to develop rheumatoid arthritis and four times more likely to have chronic fatigue syndrome than men. As a whole, autoimmune diseases, which often include debilitating pain, strike women three times more frequently than men.
While hormonal, genetic and even environmental factors might influence the manifestation and progression of autoimmune diseases, we don’t yet know the reason for this high prevalence in women.
Pain conditions are a particularly good example of the interplay between sex (our biological and chromosomal differences) and gender (the cultural roles and expectations attributed to a person). In 2011, the Institute of Medicine published a report on the public health impact of chronic pain, called “Relieving Pain in America.” It found that not only did women appear to suffer more from pain, but that women’s reports of pain were more likely to be dismissed.
This is a serious problem, because pain is subjective and self-reported, and diagnosis and treatment depend on the assumption that the person reporting symptoms is beyond doubt.
The oft-cited study “The Girl Who Cried Pain: A Bias Against Women in the Treatment of Pain” found that women were less likely to receive aggressive treatment when diagnosed, and were more likely to have their pain characterized as “emotional,” “psychogenic” and therefore “not real.”
Instead of appropriate care for physical pain, this can lead to treatment for mental health issues that might not even exist. The situation is further complicated by the fact that antidepressants are absorbed differently in women and vary in effectiveness, depending on hormonal cycles.
The routine attribution of abdominal pain from conditions like appendicitis or gastrointestinal disease to gynecological problems can also delay or complicate the diagnostic process. A 2008 study published in the journal Academic Emergency Medicine, designed to gauge gender disparities among emergency room patients complaining of abdominal pain, found that even after adjusting for race, class and triage assessment, women were still 13 to 25 percent less likely than men to receive high-strength “opioid” pain medication. Those who did get opioid pain relievers waited an average of 16 minutes longer to receive them.
Conditions like fibromyalgia or chronic fatigue syndrome, for which definitive causes have not been identified and concrete diagnostic tests are not available, illustrate the problems associated with the perceived reliability of the female patient as narrator of her pain. Women are more likely to receive diagnoses of many of these more nebulous conditions — fibromyalgia, which affects about six million patients in the United States, is nine times more likely to be diagnosed in women than in men — and this discrepancy surely contributes to the widespread skepticism that still exists over the legitimacy of these disorders.
I AM a sufferer of pain and chronic disease. Like many, I’ve had physical symptoms (in my case, respiratory problems and infections) explained away as emotional. My freshman year in college, I was in the emergency room, flanked by machines and struggling to breathe while doctors lobbed questions at me: Why wasn’t I responding to the medication the way they expected I would? Was I just too anxious? Could I not handle stress, and was that making me sick?
I was 23 before I was given a correct diagnosis of a rare genetic lung disease called primary ciliary dyskinesia. I’d been sick since birth, but long diagnostic journeys are occupational hazards of living with conditions doctors don’t often see. Still, my journey was unnecessarily protracted by my doctors’ dismissal of my symptoms as those of a neurotic young woman.
For all the medical advances of the past few decades, we still know shockingly little about pain and how to control it. Sex-based research is a crucial part of understanding not just the underlying mechanisms of pain, but the most effective ways to treat it for men and women alike. The Institute of Medicine report found gaps in research, particularly in terms of effective treatments, as well as in the oversight of pain research. The report recommended that these problems be addressed and that strategies to resolve them be implemented by 2015.
Among those improvements must be a renewed focus on discovering why women respond differently to some drugs and diseases, as well as an emphasis on training physicians to better diagnose and manage women’s pain. A report by the Campaign to End Chronic Pain in Women found that inadequate physician training in diagnosing and treating just six pain disorders that affect women either exclusively or predominantly, including fibromyalgia and chronic fatigue syndrome, added as much as $80 billion a year to America’s health care bills.
Part of the reason the diagnosis and treatment of women’s pain lag so much is simply the pace of medical research itself, which is slow to move from publication to clinical practice. Unfortunately, if anything, changes in assumptions about gender evolve even more slowly.
www.nytimes.com/2013/03/17/opinion/sunday/women-and-the-treatment-of-pain.html
Live and Learn. Learn and Live Better! is my motto. I'm Mardy Ross, and I founded Lumigrate in 2008 after a career as an occupational therapist with a background in health education and environmental research program administration. Today I function as the desk clerk for short questions people have, as well as 'concierge' services offered for those who want a thorough exploration of their health history and direction to resources likely to progress their health according to their goals. Contact Us comes to me, so please do if you have questions or comments. Lumigrate is "Lighting the Path to Health and Well-Being" for increasing numbers of people. Follow us on social networking sites such as: Twitter: http://twitter.com/lumigrate and Facebook. (There is my personal page and several Lumigrate pages. For those interested in "groovy" local education and networking for those uniquely talented LumiGRATE experts located in my own back yard, "LumiGRATE Groove of the Grand Valley" is a Facebook page to join. (Many who have joined are beyond our area but like to see the Groovy information! We not only have FUN, we are learning about other providers we can be referring patients to and 'wearing a groove' to each other's doors -- or websites/home offices!) By covering some of the things we do, including case examples, it reinforces the concepts at Lumigrate.com as well as making YOU feel that you're part of a community. Which you ARE at Lumigrate!
This forum is provided to allow members of Lumigrate to share information and ideas. Any recommendations made by forum members regarding medical treatments, medications, or procedures are not endorsed by Lumigrate or practitioners who serve as Lumigrate's medical experts.


![Expand cart block. []](/sites/all/modules/ubercart/uc_cart/images/bullet-arrow-up.gif)